
Better Care Management: A Performance Review
03/14/2023
Over the past months, we used these pages to share insights on matters of interest and concern to health benefit plan leaders. We have described approaches for addressing complex, high-cost health problems, and reviewed the steps we walked with our plan participants to improve their lives and reduce their healthcare costs.
We will do more of that, for there is much more to share.
You, our reader, however, may want to know (should want to know) more about how this is working. So that is the point of this blog/entry/piece today—a performance review, of sorts.
Here’s a snapshot of recent activity: Two major clients, two customized, personalized approaches following a similar set of proven principles:
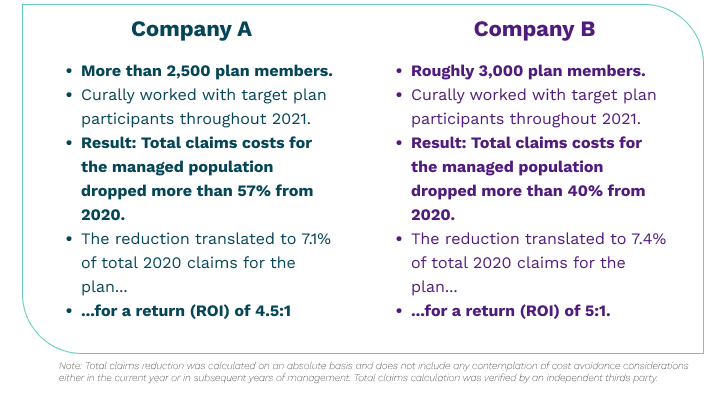
That’s a glance at substantive, quantifiable success with healthcare management–achieving returns on investment (ROI) of 4.5 to 1 and 5 to 1, respectively.
It is not the entire picture, however, as it does not include the reduced absenteeism and increased productivity we hear about from employers seeing healthier, happier employees at work. (Perhaps that is a measure we will be able to present in a future review.)
Less quantifiable, but equally important in our work with plan participants, is the reduction in disease burden and improvement in their quality of life. We haven’t found a way to put it in a chart, but we know it’s there—our nurses see it regularly in the smiles and in the stories of our participants and their families. We shared a few of these stories already (Marie’s story and John’s story are examples). You will be seeing more of these as we go forward.
Knowing the source of the success
Most of what we do is condition management, but it is likely not the condition management others talk about.
The biggest misunderstanding we face in our work results from the imprecise application of the labels “care management” or “case management” or “condition management” by insurers, providers and others. Employers will hear any of these terms and assume they already have that. And they may, but it is likely not what Curally provides. The difference can be a matter of both degree and commitment.
We took years of experience and insights from the medical and employee health benefits worlds to develop our approach for reducing the burden of illness and cost plaguing large health benefit plans. We created tools and processes that help us work effectively. That’s important, but it is not enough.
Recent studies have concluded that 31 percent of US healthcare costs can be attributed directly to “behaviorally influenced chronic conditions,” while 69 percent of costs are influenced by consumer behaviors.
So we went further, making a huge commitment to helping individual plan participants understand their health conditions, embrace their treatment plans and actually change their behaviors for the better.
This is difficult work, but it has the biggest payoff.
Once we identify the plan participants facing the biggest health challenges and risks, we confidentially reach out to them. We have a team of exceptional nurses who can do it—each demonstrating toughness with compassion, love and care. They train, they coach, they step in to help the participant overcome obstacles, and they do a lot of listening.
The nurses are supported by a highly skilled and knowledgeable physician, and everybody is working not to change the individual plan participants but to help the participants change themselves.
Importantly, we meet plan participants where they are, how and where they are most comfortable. It takes a personalized, compassionate and unrelenting effort. Chronic conditions are stubborn things. We have to be tenacious in our response.
For individuals with more complex and high-cost cases, we serve as advocates and coordinators, working with treating providers to ensure seamless care consistent with high medical standards. Where appropriate, we will work with the participant to transition their care to make sure their needs are met.
That’s the substantive sauce of success. (Nothing secret here, which is why we are willing to share it openly.) It is application of know-how built from experience and a proven approach.
You know now from Marie’s and John’s stories (referenced above) how this looks at the participant level. There are many more examples, such as the case of the woman with metastatic cancer whose treatment was falling short. Our Chief Medical Officer challenged the existing treatment protocol, which involved long-term, expensive therapies designed to stabilize the disease.
After an extensive review of her medical records, Dr. Vesta encouraged the participant to consider a surgical procedure from an out-of-network provider, a different approach that had the strong potential to be curative. The result was remarkable, as the participant continues to be in remission and is not currently receiving chemotherapy or other cancer specialty drugs.
These are just a few of the successes achieved through our approach and people.
Getting Started is Easy
Like chronic conditions, the status quo is stubborn. Making significant change is hard. We do everything we can to make it easy, for we do nearly all the work. All we need from the employers we work with is claims data and the authorization to proceed.
We design our customized plans taking into account the organization’s culture as well as historical challenges and current concerns the employer wants to address.
We prepare, with the organization’s leadership, an effective program rollout and employee communication plan.
Within the first three months, we are running at full capacity, engaging with participants and making progress toward their personalized individual goals.
Our Review, Like Our Work, Is Ongoing
